What Is Patient First ESKD Life-Plan?
- It is a strategy that should start early in the pre-dialysis period and encompasses a continuum-of-care model for chronic kidney disease.
- It maps out an individualised plan for kidney replacement therapy modalities for a patient; in doing so, the dialysis access strategy is optimally considered.

When Is The Appropriate Timing For Kidney Replacement Therapy (KRT) Planning?
- Early KRT planning is essential to prevent unwanted ‘crash-landing’ dialysis initiation which carries significant short- and long-term complications.
- A patient with eGFR < 30 - 45 mL/min/1.73 m² should be referred to nephrologist for comprehensive review. KRT planning should be initiated when eGFR 15-20 mL/min/1.73 m².
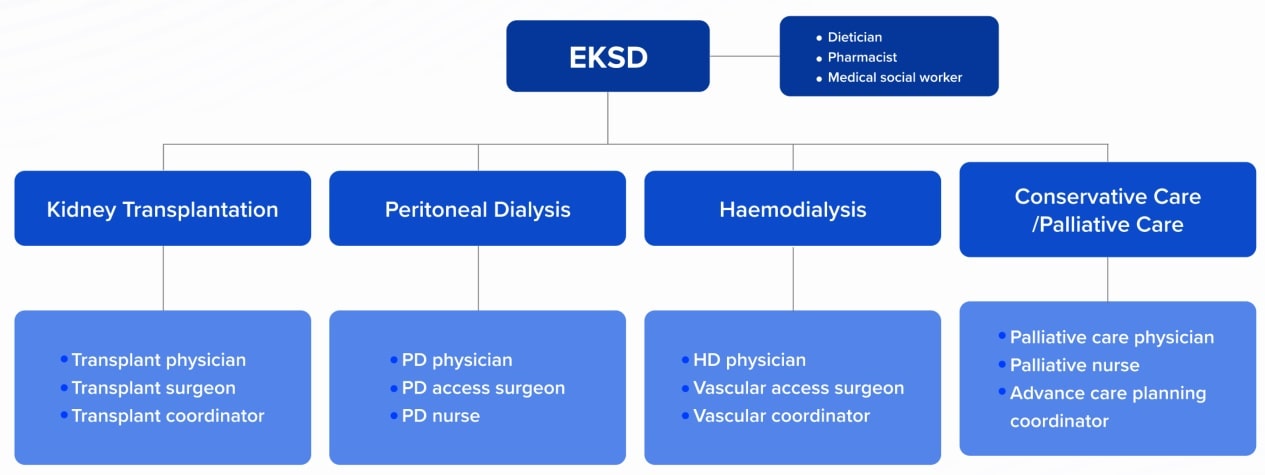
Kidney Replacement Therapy Planning: A Multidisciplinary Approach
What Is Dialysis Access?
- Dialysis access is the ‘life-line’ of ESKD patient.
- It comprises peritoneal dialysis (PD) catheter, central venous catheter (CVC), arteriovenous fistula (AVF) and arteriovenous graft (AVG).
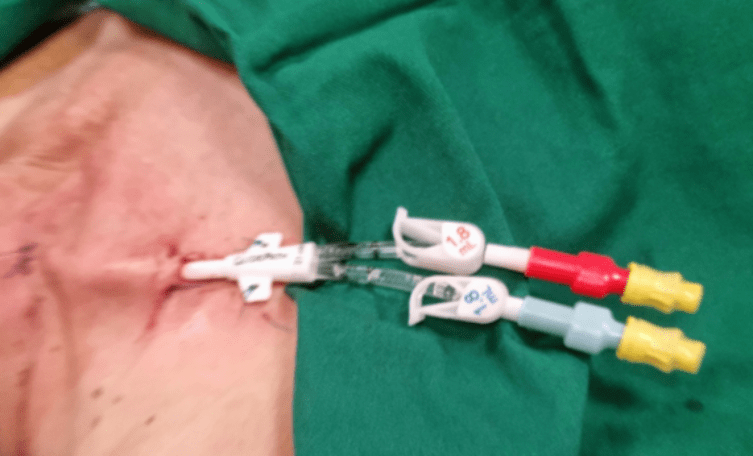
Central Venous Catheter (CVC)
The haemodialysis catheter conundrum: Hate living with them, but can’t live without them.
Steve J. Schwab and Gerald Beathard. Kidney International; 1999: 56, 1–17
- CVCs are generally used as a temporary access, but sometimes they are permanent.
Its use is generally associated with higher short- and long-term complications. - Haemodialysis initiation with CVC i.e. ‘crash-landing’ is discouraged.
Indications For Short-Term HD CVC
- Acute kidney injury requiring kidney replacement therapy.
- Bridging measures for AVF/AVG, PD and transplant complications.
- Dialysis initiation before living donor kidney transplantation < 90 days.
- ‘Crash-landing’ dialysis initiation.
Indications For Long-Term HD CVC
- No other AV access or PD option available.
- Limited life-expectancy (e.g. frail elderly, advanced cancer or poor cardiac reserve).
- Poor quality of life.
Tunnelled Cuffed CVC
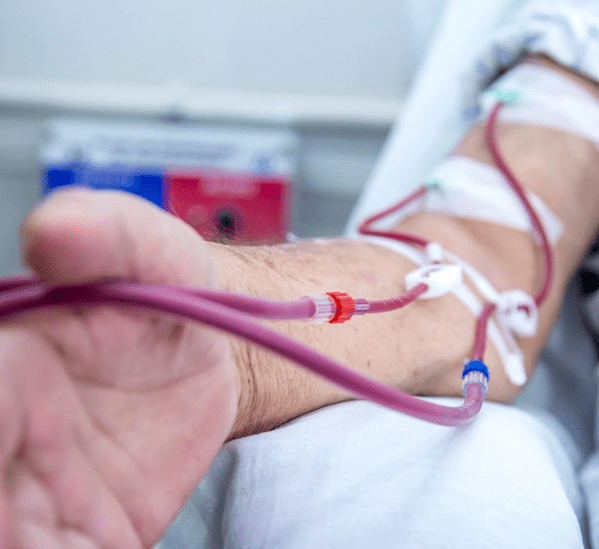
Arteriovenous Fistula (AVF)
- An AVF should be considered the first choice for HD access because it generally lasts longer and has fewer problems such as infections and clotting.
- It is surgically created by joining a suitable artery and vein.
- As there is a need of minimal 6 – 8 weeks for maturation, AVF should be created early before HD initiation.
Arteriovenous Graft (AVG)
- Some patients may not be able to receive an AVF because their blood vessels are too small.
- An AVG is considered the second choice for an access.
- It is surgically created by using a piece of synthetic tube to join an artery and vein.
Caring For Dialysis Access
- Whether your access is a CVC, AVF or AVG, you must take good care of it.
- Your dialysis care team will teach you the steps of optimal access care.
- Your dialysis care team will examine and monitor your access to make sure it is working well.
If you are having AVF or AVG, here are some tips you should follow to keep your access working longer: Check the blood flow few times each day by feeling for a vibration, also called a thrill. If there is a change or absent, call your doctor or your dialysis centre immediately.
- Do not wear tight clothes or jewellery on your access arm.
- Do not sleep with your head on your access arm.
- Do not let anyone use a blood pressure cuff on your access arm.
- Do not let anyone draw blood from your access arm.
- Do not be afraid to ask your dialysis care team to rotate the needle sites.
- Apply only gentle pressure to the access site after the needle is removed.
- If you have breakthrough bleeding after you have dialysis, apply gentle pressure to the needle site with a clean towel or gauze pad.
- If the bleeding does not stop in 30 minutes, call your doctor or your dialysis centre immediately.
Dialysis Access Emergency
Please contact your doctor or dialysis centre immediately, or proceed to emergency department of your hospital if you have the issues below:
- No thrill or bruit: clotted access
- Unexpected or prolonged bleeding at the access site
- Broken catheter
- Pus from the catheter exit site
- Shinny, thin skinned and pulsatile aneurysm
- Redness, swelling or pain of the access site
References
1. KDOQI clinical practice guidelines for vascular access: 2019 update. Am J Kidney Dis. 2020;75(4)(suppl 2):S1-S164.
2. https://www.youtube.com/watch?v=sUQryu5myHI



